On April 23, the Centers for Medicare and Medicaid Services (CMS) published its minimum staffing rule for skilled nursing facilities (SNFs). Operators and stakeholders have waited in anticipation to see what the final rule would look like and how it might impact their operations and the industry. The rule is largely similar to the proposed version but has some key differences outlined in the table below.
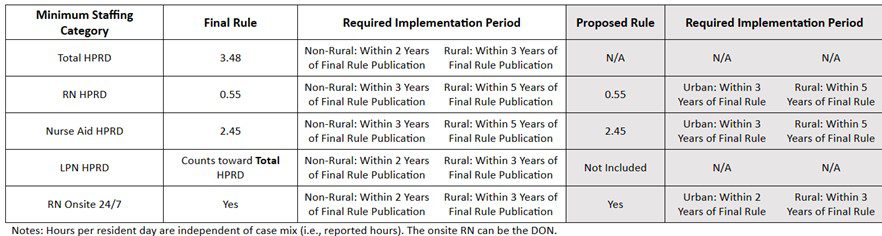
In the final rule, CMS implemented their proposal to require 24/7 registered nurse (RN) coverage and, separately, at least 0.55 hours per resident day (HPRD) of RN time and 2.45 HPRD of nurse aide time. The director of nursing (DON) can count toward the RN requirements if the DON is available to provide direct resident care. They have also added an overall requirement of 3.48 HPRD of total direct nurse staffing requirements which RNs, licensed practical nurses, or nurse aides can fill.
As noted by the American Health Care Association (AHCA), a potentially positive change in the final rule is a temporary exemption from the staffing requirements. CMS added the exemption to the pre-existing nurse staffing waivers that have not proven useful over the years. The exemption can excuse a facility from eight hours of the 24/7 RN requirement and any or all the HPRD standards. The exemption appears to be difficult to obtain, despite CMS’s suggestion that 25% of the SNFs in the country could qualify. A few of the major requirements for the exemption include:
- The facility has a survey and is cited for not meeting one or more of the staffing requirements.
- The facility has not been cited for an H-level or higher staffing deficiency within the past 12 months.
- The facility is not a special focus facility.
- The facility can prove it is engaging in active recruiting, paying competitive wages, and dedicating sufficient resources to staffing.
The staffing rule only has one component that takes effect in the next few months, specifically on August 8, 2024. This component includes a set of changes to the annual facility assessment requirements, requiring each facility to have a plan in place to address some of the following:
- Resources necessary to care for its residents competently during both day-to-day operations and emergencies
- Care requirements to meet the needs of different patient populations within the facility
- Staff competencies and ongoing training requirements in addition to meeting mandatory staffing levels through recruitment and retention
- Physical environment necessary to care for its patient population
- Building, equipment, and contracted services to meet the needs of all patients being served
CMS plans to assess compliance with staffing requirements by reviewing both state survey results and facility payroll data. The enforcement of the minimum staffing rule is still under consideration. CMS has indicated that additional regulatory guidance will be issued closer to the effective date of each provision of the rule, which will provide more information on survey and enforcement details.
The implementation dates in the final rule are differentiated by non-rural and rural status. For non-rural facilities, the 24/7 RN and 3.48 total HPRD requirements apply two years after the rule is published in the Federal Register (May 10, 2026), while those same standards apply three years after publication (May 10, 2027) for rural facilities. The 0.55 RN and 2.45 nurse aide HPRD requirements apply three years after publication (May 10, 2027) for non-rural facilities and 5 years after publication (May 10, 2029) for rural facilities. Based on consideration of comments, CMS adopted the OMB definition of “rural” in the finalized rule.
The most important thing to know now is the major regulatory components do not take effect for two to five years. Operators and opponents of the legislation are cautiously optimistic that those requirements may never apply because the AHCA and other advocates are engaging in an all-out legislative and legal effort to stop the rule from ever being implemented. That said, being aware of the proposed changes is critical, as this is an issue that will continue to develop in the coming months and years.
During a recent acquisition financing, Lument’s operational and staffing expertise helped a SNF improve its bottom line. Read more in this case study.

